The Surprising Ways Gluten Impacts Your Skin: From Rashes to Radiance
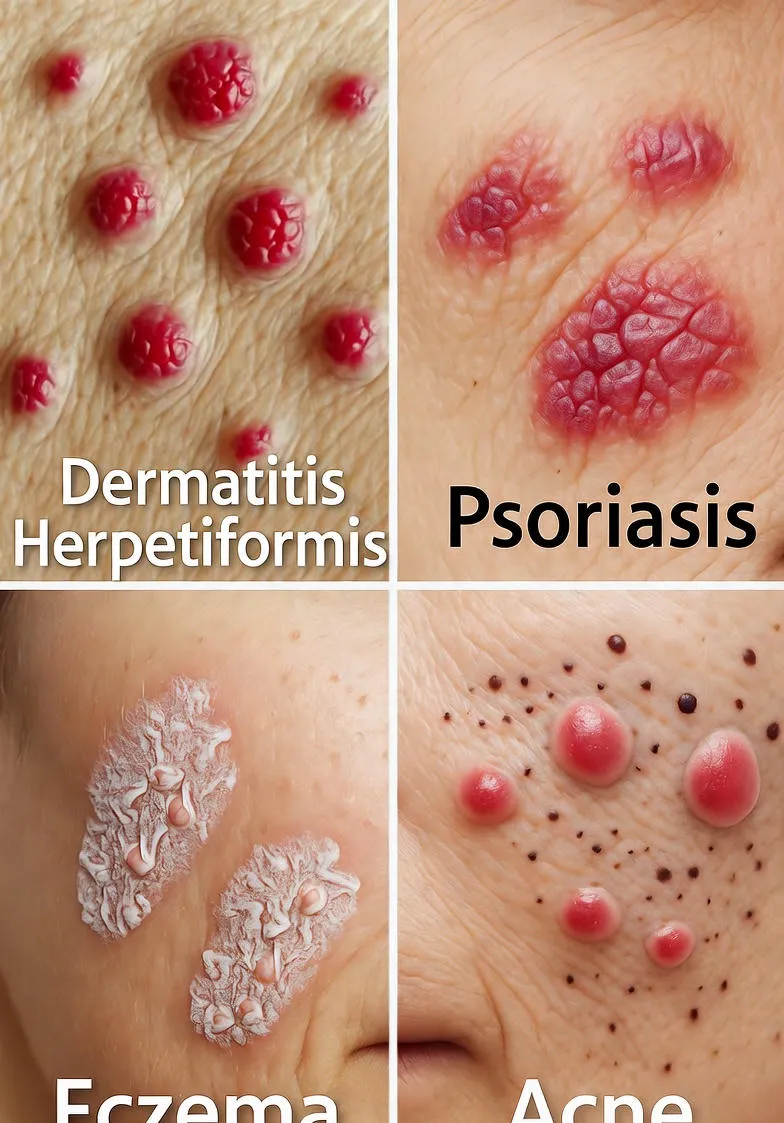
Explore the hidden effects of gluten on skin health, including dermatitis herpetiformis, psoriasis, eczema, and acne. Learn how a gluten-free diet can transform your skin via the gut-skin connection.
Introduction
Have you ever wondered why your skin seems to rebel with unexplained rashes, persistent acne, or itchy flare-ups, even after trying every cream and lotion under the sun? The culprit might be hiding in your pantry: gluten. This common protein found in wheat, barley, and rye has long been associated with digestive woes, but its effects on the skin are only recently gaining the spotlight they deserve. For millions suffering from gluten-related disorders, the connection between what they eat and how their skin looks and feels is profound. In this comprehensive guide, we'll dive deep into the effects of gluten on skin health, exploring everything from severe autoimmune reactions to subtler inflammatory responses. Whether you're dealing with celiac disease or simply suspecting a sensitivity, understanding this link could be the key to unlocking clearer, calmer skin.
Gluten's influence on the skin isn't just anecdotal; it's backed by a growing body of research highlighting the intricate gut-skin axis. When gluten triggers an immune response in sensitive individuals, it can cascade into widespread inflammation, manifesting as everything from blistering rashes to chronic dryness. But there's hope: adopting a gluten-free lifestyle has transformed the skin of countless people, reducing symptoms and restoring balance. As we unpack the science, symptoms, and solutions, you'll gain the knowledge to assess if gluten is sabotaging your skin—and what to do about it.
What is Gluten and Why Does It Matter?
Gluten is a group of proteins that act like glue, giving dough its elasticity and baked goods their chewiness. It's a staple in modern diets, lurking in bread, pasta, cereals, and even processed foods like sauces and soups. For most people, gluten passes through the digestive system without issue, but for those with celiac disease or non-celiac gluten sensitivity, it sparks a cascade of problems.
In the gut, gluten can damage the intestinal lining in susceptible individuals, leading to leaky gut syndrome. This permeability allows undigested food particles and toxins to enter the bloodstream, prompting systemic inflammation. The skin, as the body's largest organ and a primary detox pathway, often bears the brunt of this turmoil. Studies show that up to 10-15% of people with celiac disease experience skin manifestations, underscoring gluten's far-reaching impact beyond the belly.
Gluten and Celiac Disease: The Autoimmune Connection
Celiac disease affects about 1% of the global population, an autoimmune disorder where ingesting gluten prompts the immune system to attack the small intestine. This attack impairs nutrient absorption, leading to deficiencies in vitamins like A, D, E, and zinc—all crucial for skin health. Without these nutrients, skin can become dry, scaly, and prone to infections.
Beyond malabsorption, the chronic inflammation from celiac disease fuels oxidative stress, accelerating aging and exacerbating conditions like wrinkles and hyperpigmentation. Research from the National Institutes of Health indicates that untreated celiac patients often report skin complaints as their first noticeable symptoms, sometimes years before gut issues surface. Addressing the root cause—gluten—can reverse these effects, but early diagnosis is key to preventing long-term damage.
Dermatitis Herpetiformis: The Hallmark Skin Rash of Gluten Sensitivity
Among the most direct effects of gluten on the skin is dermatitis herpetiformis (DH), often called the 'gluten rash.' This intensely itchy condition features clusters of small blisters and bumps, typically on the elbows, knees, buttocks, scalp, and back. Caused by gluten-triggered IgA antibodies depositing in the skin, DH is virtually synonymous with celiac disease—nearly all sufferers have the intestinal form, even if undiagnosed.
Symptoms can be debilitating, with burning and stinging that disrupts sleep and daily life. The rash waxes and wanes with gluten exposure, sometimes appearing within hours of consumption. Diagnosis involves a skin biopsy showing IgA deposits, alongside blood tests for celiac antibodies. Treatment? A strict gluten-free diet, which can clear the rash in weeks to months, though some may need dapsone medication for itch relief. The Celiac Disease Foundation notes that up to 25% of celiac patients develop DH, making it a critical red flag for gluten intolerance.
Gluten's Role in Psoriasis and Plaque Buildup
Psoriasis, a chronic autoimmune condition causing red, scaly plaques, has a surprising link to gluten. Studies, including those from the Journal of the American Academy of Dermatology, reveal higher rates of celiac disease among psoriasis patients. Even without full-blown celiac, gluten can exacerbate plaques by promoting pro-inflammatory cytokines like TNF-alpha.
Adopting a gluten-free diet has led to significant improvements in up to 50% of sensitive psoriasis sufferers, with reduced scaling and fewer flares. The mechanism ties back to the gut: gluten-induced dysbiosis alters the microbiome, sending inflammatory signals to the skin via the bloodstream. If your psoriasis stubbornly resists topicals, testing for gluten sensitivity could be a game-changer.
Eczema and the Itch That Won't Quit
Eczema, or atopic dermatitis, plagues millions with dry, inflamed, and unbearably itchy skin. While not directly caused by gluten, research from Healthline and Medical News Today suggests that for those with non-celiac gluten sensitivity, wheat proteins can trigger flares. This is especially true in children, where eczema co-occurs with food sensitivities at rates up to 30%.
The connection? Gluten may heighten histamine release and Th2 immune responses, worsening barrier function and inviting allergens. A 2023 NIH review found that anti-gliadin IgA antibodies correlate with eczema severity, hinting at gluten's role. Eliminating it often soothes symptoms within 4-6 weeks, complementing moisturizers and steroids for holistic relief.
Acne: When Gluten Fuels Breakouts
Acne isn't just a teenage rite of passage; for adults, it can signal deeper imbalances. Gluten enters the picture through insulin spikes: refined wheat products raise blood sugar, boosting oil production and pore-clogging. In gluten-sensitive folks, added inflammation from leaky gut amplifies this, leading to cystic, hormonal acne.
A study in the Journal of Clinical and Aesthetic Dermatology linked gluten-free diets to clearer skin in non-celiac patients, attributing it to reduced IGF-1 hormone levels. If dairy and sugar tweaks haven't helped your breakouts, scrutinizing gluten could reveal the missing link.
Other Skin Concerns: From Hair Loss to Dryness
Gluten's tentacles extend to alopecia areata, an autoimmune hair loss condition with elevated celiac prevalence. Gluten-free adherence has regrown hair in responsive cases. Chronic dryness and keratosis pilaris—those bumpy arms—may stem from nutrient malabsorption, while vitiligo and urticaria (hives) occasionally flare with gluten challenges.
Even rosacea, the facial redness beast, shows anecdotal ties, with some reporting calmer cheeks post-elimination. These subtler effects highlight gluten's broad inflammatory footprint, urging a holistic view of diet and dermatology.
The Science Behind the Gut-Skin Axis
At the heart of gluten's skin sabotage is the gut-skin axis, a bidirectional communication highway. Poor gut health from gluten leaks endotoxins, activating skin mast cells and keratinocytes for inflammation. Probiotics and prebiotics can modulate this, but first, remove the trigger.
Emerging research on the skin microbiome reveals gluten's disruption of bacterial balance, mirroring gut dysbiosis. This fosters overgrowth of inflammatory species, perpetuating cycles of irritation. Understanding this empowers targeted interventions beyond mere avoidance.
Diagnosing Gluten-Related Skin Issues
Suspecting gluten's hand? Start with blood tests for tTG-IgA and anti-gliadin antibodies, followed by an intestinal biopsy for celiac confirmation. For non-celiac sensitivity, an elimination diet—gluten-free for 4-6 weeks, then reintroduction—reveals reactions. Track skin changes in a journal for patterns.
Consult a dermatologist or gastroenterologist; self-diagnosis risks nutritional pitfalls. Genetic testing for HLA-DQ2/DQ8 flags predisposition, guiding proactive steps.
Embracing a Gluten-Free Diet for Glowing Skin
Going gluten-free isn't deprivation; it's liberation for your skin. Expect initial detox symptoms, but soon comes relief: diminished rashes, evened tone, and vitality. Nutrient-dense alternatives like quinoa, almond flour, and fresh produce fill the void, boosting collagen and antioxidants.
Clinical trials show 70-80% symptom improvement in DH patients within months. For milder issues, skin clarity enhances as inflammation ebbs, revealing the true you underneath.
Practical Tips for a Seamless Transition
- Read Labels Religiously: Gluten hides in 'modified food starch' and malt.
- Stock Up Smart: Oats (certified GF), rice, and buckwheat are safe bets.
- Meal Prep Mastery: Batch-cook salads and stir-fries for effortless eating.
- Dine Out Savvy: Apps like Find Me Gluten Free spotlight safe spots.
- Supplements Support: Probiotics and omega-3s aid gut healing.
- Skin Synergy: Pair diet with gentle cleansers and hyaluronic acid.
Conclusion
The effects of gluten on skin are a testament to diet's profound power over our largest organ. From the blistering agony of dermatitis herpetiformis to the stubborn persistence of acne and eczema, gluten can be a silent saboteur. Yet, awareness and action—through diagnosis and a gluten-free pivot—offer redemption. Imagine waking to itch-free mornings, breakout-free mirrors, and skin that radiates health. It's not just possible; it's probable for those who listen to their body's whispers. Consult professionals, experiment mindfully, and let your skin thank you with every smooth touch. Your journey to gluten-free glow starts now.


